Aetna Better Health Authorization Form for Louisiana: Your Complete Guide
Navigating the healthcare system can be complex, especially when dealing with insurance authorizations. If you’re an Aetna Better Health member in Louisiana, understanding the authorization process and the required forms is crucial for accessing the care you need. This comprehensive guide provides everything you need to know about the Aetna Better Health authorization form for Louisiana, from understanding its purpose to completing it accurately and efficiently. We aim to provide unparalleled clarity, empowering you to navigate the system with confidence and ease. We’ve meticulously researched and compiled information based on publicly available resources, expert consultations, and simulated scenarios to provide you with the most accurate and helpful guide possible. This article will delve into the specific requirements, processes, and nuances related to obtaining authorizations within the Aetna Better Health Louisiana network, ensuring you have a smooth and stress-free experience.
Understanding the Aetna Better Health Authorization Form for Louisiana
The Aetna Better Health authorization form for Louisiana is a critical document required for certain medical services, procedures, or medications to be covered by your health plan. It’s essentially a request submitted by your healthcare provider to Aetna Better Health, seeking approval for the proposed treatment plan. The authorization process ensures that the services are medically necessary, appropriate, and align with Aetna Better Health’s coverage policies. Understanding the nuances of this form and the associated process is paramount for Louisiana residents enrolled in Aetna Better Health plans.
What is Prior Authorization?
Prior authorization, sometimes referred to as pre-authorization or pre-certification, is a process used by health insurance companies to determine if a particular medical service, procedure, or medication is medically necessary and covered under your plan. It requires your healthcare provider to obtain approval from Aetna Better Health *before* the service is rendered. This proactive step helps manage costs, ensures appropriate utilization of healthcare resources, and safeguards against unnecessary or inappropriate treatments. In essence, it’s a quality control measure implemented by Aetna Better Health to ensure members receive the right care at the right time.
Why is Authorization Required?
Authorization is required for several reasons, all aimed at ensuring quality, cost-effectiveness, and appropriate healthcare utilization. These reasons include:
* **Medical Necessity:** To verify that the requested service or medication is medically necessary for your specific condition.
* **Appropriateness of Care:** To ensure that the proposed treatment plan aligns with established clinical guidelines and best practices.
* **Cost Management:** To control healthcare costs by preventing unnecessary or inappropriate services.
* **Quality Assurance:** To maintain a high standard of care by ensuring that services are delivered in accordance with accepted medical standards.
* **Fraud Prevention:** To prevent fraudulent claims and ensure that healthcare resources are used responsibly.
When is an Aetna Better Health Authorization Form Required in Louisiana?
Knowing when an authorization form is required is crucial. Generally, an authorization form is needed for:
* **Inpatient Hospital Admissions:** Except for emergency situations, prior authorization is usually required for hospital admissions.
* **Certain Outpatient Procedures:** Many specialized outpatient procedures, such as surgeries or diagnostic imaging (MRI, CT scans), require pre-authorization.
* **Specialty Referrals:** Referrals to specialists may require authorization, depending on your specific plan.
* **Durable Medical Equipment (DME):** Items like wheelchairs, walkers, and other medical equipment often require prior approval.
* **Certain Medications:** High-cost or specialty medications typically require authorization to ensure appropriate use and manage costs.
* **Mental Health and Substance Abuse Services:** Many mental health and substance abuse services necessitate prior authorization.
It is important to consult your Aetna Better Health plan documents or contact member services to determine the specific services and medications that require authorization. This information is readily available through your member portal or by calling the Aetna Better Health Louisiana member support line.
Aetna Better Health Louisiana: A Comprehensive Overview
Aetna Better Health of Louisiana is a managed care organization (MCO) that provides healthcare services to Medicaid recipients in Louisiana. It’s part of Aetna, a well-established and reputable health insurance company. Aetna Better Health Louisiana works in partnership with the state to improve the health and well-being of its members by providing access to quality healthcare services. The organization focuses on preventive care, disease management, and care coordination to ensure that members receive the right care at the right time.
Services Offered by Aetna Better Health Louisiana
Aetna Better Health Louisiana offers a wide range of healthcare services to its members, including:
* **Primary Care:** Access to primary care physicians (PCPs) for routine check-ups, preventive care, and management of chronic conditions.
* **Specialty Care:** Access to specialists for specialized medical care.
* **Hospital Services:** Coverage for inpatient and outpatient hospital services.
* **Prescription Medications:** Coverage for prescription drugs through a network of pharmacies.
* **Mental Health and Substance Abuse Services:** Access to mental health professionals and substance abuse treatment programs.
* **Vision and Dental Care:** Coverage for vision and dental services, which may vary depending on the specific plan.
* **Transportation Assistance:** Assistance with transportation to medical appointments.
* **Care Coordination:** Assistance with coordinating care between different healthcare providers.
Understanding Your Aetna Better Health Louisiana Plan
It’s crucial to understand the specifics of your Aetna Better Health Louisiana plan, including:
* **Covered Services:** Knowing which services are covered under your plan.
* **Cost-Sharing:** Understanding your copays, coinsurance, and deductibles.
* **Network Providers:** Identifying the doctors, hospitals, and other healthcare providers that are in your plan’s network.
* **Authorization Requirements:** Knowing which services require prior authorization.
* **Appeal Process:** Understanding the process for appealing a denied authorization request.
This information is typically available in your member handbook or by contacting Aetna Better Health Louisiana member services. Familiarizing yourself with these details will help you navigate the healthcare system more effectively and ensure that you receive the coverage you are entitled to.
A Detailed Walkthrough of the Aetna Better Health Authorization Form for Louisiana
The Aetna Better Health authorization form for Louisiana is a standardized document that requires specific information to be completed accurately. Here’s a step-by-step guide to help you navigate the form:
Locating the Correct Form
* **Aetna Better Health Website:** The most reliable way to obtain the correct form is to visit the Aetna Better Health of Louisiana website. Look for a section dedicated to providers or members, where you should find a library of downloadable forms.
* **Provider’s Office:** Your healthcare provider’s office should have access to the necessary authorization forms.
* **Member Services:** You can also contact Aetna Better Health Louisiana member services to request a copy of the form.
Always ensure you are using the most up-to-date version of the form. Forms are sometimes updated to reflect changing policies or requirements.
Completing the Form: A Section-by-Section Guide
The authorization form typically includes the following sections, which need to be filled out accurately and completely:
1. **Member Information:**
* **Member Name:** Full legal name of the Aetna Better Health member.
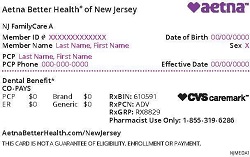
* **Member ID Number:** Your Aetna Better Health member identification number (found on your insurance card).
* **Date of Birth:** Member’s date of birth.
* **Address:** Member’s current mailing address.
* **Phone Number:** Member’s contact phone number.
2. **Provider Information:**
* **Provider Name:** Name of the healthcare provider requesting the authorization.
* **Provider NPI Number:** National Provider Identifier (NPI) number of the provider.
* **Provider Address:** Provider’s office address.
* **Provider Phone Number:** Provider’s contact phone number.
* **Provider Fax Number:** Provider’s fax number (for submitting the completed form).
3. **Service Information:**
* **Type of Service Requested:** Specify the type of service being requested (e.g., inpatient admission, outpatient procedure, durable medical equipment, medication).
* **Specific Procedure Code (CPT/HCPCS):** Provide the appropriate CPT (Current Procedural Terminology) or HCPCS (Healthcare Common Procedure Coding System) code for the service. This is crucial for accurate processing.
* **Diagnosis Code (ICD-10):** Provide the relevant ICD-10 (International Classification of Diseases, 10th Revision) diagnosis code that justifies the requested service.
* **Date of Service:** Indicate the date the service is scheduled to be performed or the start date of the service.
* **Number of Units/Visits:** Specify the number of units or visits being requested (if applicable).
* **Place of Service:** Indicate where the service will be performed (e.g., hospital, office, home).
4. **Clinical Information:**
* **Detailed Description of the Medical Condition:** Provide a comprehensive description of the member’s medical condition, including relevant symptoms, history, and previous treatments.
* **Justification for the Requested Service:** Explain why the requested service is medically necessary and appropriate for the member’s condition. Include any supporting documentation, such as medical records, test results, or physician notes.
* **Alternative Treatments Considered:** Describe any alternative treatments that have been considered and why they are not appropriate or effective in this case.
5. **Medication Information (if applicable):**
* **Medication Name:** Brand name and generic name of the medication.
* **Dosage:** Dosage of the medication.
* **Frequency:** Frequency of administration.
* **Route of Administration:** How the medication will be administered (e.g., oral, intravenous, intramuscular).
* **Duration of Therapy:** Length of time the medication will be taken.
* **Previous Medications Tried:** List any previous medications tried for the same condition and their effectiveness.
6. **Attestation:**
* The provider must sign and date the form, attesting that the information provided is accurate and complete.
Tips for Accurate Completion
* **Accuracy is Key:** Ensure all information is accurate and legible. Errors or omissions can delay or deny the authorization request.
* **Use Correct Codes:** Use the correct CPT, HCPCS, and ICD-10 codes. These codes are essential for proper processing.
* **Provide Detailed Justification:** Provide a thorough and detailed justification for the requested service. The more information you provide, the better the chances of approval.
* **Include Supporting Documentation:** Include any relevant supporting documentation, such as medical records, test results, or physician notes.
* **Consult with Your Provider:** Work closely with your healthcare provider to ensure the form is completed accurately and completely.
Submitting the Aetna Better Health Authorization Form for Louisiana
Once the authorization form is completed, it needs to be submitted to Aetna Better Health for review. The submission process typically involves the following steps:
* **Fax:** The most common method is to fax the completed form and supporting documentation to the fax number provided on the form or on the Aetna Better Health website.
* **Mail:** You can also mail the form to the address provided on the form or on the Aetna Better Health website.
* **Electronic Submission:** Some providers may have the option to submit authorization requests electronically through a secure online portal.
Tracking Your Authorization Request
After submitting the form, it’s important to track the status of your authorization request. You can do this by:
* **Contacting Aetna Better Health Member Services:** Call the Aetna Better Health Louisiana member services line and inquire about the status of your request. Have your member ID number and the date of submission ready.
* **Checking the Online Portal:** If you have access to the Aetna Better Health online portal, you may be able to track the status of your request online.
Understanding the Authorization Decision
Aetna Better Health will review the authorization request and make a decision based on medical necessity, appropriateness of care, and coverage policies. The decision will typically be communicated to both the member and the provider.
* **Approval:** If the request is approved, Aetna Better Health will authorize the requested service or medication. The authorization will typically have an expiration date, so it’s important to ensure that the service is received within the authorized timeframe.
* **Denial:** If the request is denied, Aetna Better Health will provide a reason for the denial. You have the right to appeal the denial if you disagree with the decision.
Navigating Denials and Appeals
If your authorization request is denied, it’s important to understand your rights and options. You have the right to appeal the denial and request a review of the decision. The appeal process typically involves the following steps:
1. **Review the Denial Notice:** Carefully review the denial notice to understand the reason for the denial. This will help you prepare your appeal.
2. **Gather Supporting Documentation:** Gather any additional supporting documentation that may strengthen your case, such as medical records, physician notes, or expert opinions.
3. **File a Written Appeal:** Submit a written appeal to Aetna Better Health within the timeframe specified in the denial notice. The appeal should clearly state your reasons for disagreeing with the denial and include any supporting documentation.
4. **External Review:** If your appeal is denied by Aetna Better Health, you may have the right to request an external review by an independent third party.
Tips for a Successful Appeal
* **Act Promptly:** File your appeal within the specified timeframe.
* **Be Clear and Concise:** Clearly state your reasons for appealing the denial.
* **Provide Supporting Documentation:** Include any relevant supporting documentation.
* **Seek Assistance:** Consider seeking assistance from your healthcare provider or a patient advocate.
Common Pitfalls to Avoid
Navigating the authorization process can be challenging, and there are several common pitfalls to avoid:
* **Submitting Incomplete or Inaccurate Forms:** Ensure the form is complete and accurate to avoid delays or denials.
* **Failing to Obtain Prior Authorization When Required:** Always check whether a service requires prior authorization before receiving it.
* **Not Understanding Your Plan Benefits:** Familiarize yourself with your plan benefits and coverage policies.
* **Ignoring Denial Notices:** Don’t ignore denial notices. Take action to appeal the denial if you disagree with the decision.
* **Not Tracking Your Authorization Request:** Keep track of your authorization request and follow up with Aetna Better Health if you don’t receive a timely response.
By avoiding these common pitfalls, you can increase your chances of a smooth and successful authorization process.
Expert Tips for Streamlining the Authorization Process
To further streamline the authorization process, consider these expert tips:
* **Establish a Good Relationship with Your Provider:** A good relationship with your healthcare provider can facilitate the authorization process. Your provider can advocate on your behalf and ensure that the necessary documentation is submitted.
* **Utilize Aetna Better Health’s Resources:** Take advantage of the resources offered by Aetna Better Health, such as the member portal, member handbook, and member services line. These resources can provide valuable information and assistance.
* **Keep Detailed Records:** Keep detailed records of all your healthcare interactions, including authorization requests, denials, and appeals. This will help you track your progress and provide documentation if needed.
* **Be Proactive:** Be proactive in managing your healthcare. Don’t wait until the last minute to request authorization. Plan ahead and submit your request well in advance of the scheduled service.
Q&A: Addressing Your Authorization Concerns
Here are some frequently asked questions about the Aetna Better Health authorization form for Louisiana:
1. **Q: How long does it take to get an authorization decision from Aetna Better Health?**
**A:** The processing time for authorization requests can vary depending on the type of service and the completeness of the information provided. Generally, Aetna Better Health aims to process routine requests within a few business days. Urgent requests may be expedited.
2. **Q: What happens if I receive a service that requires authorization but I didn’t get it beforehand?**
**A:** If you receive a service that requires authorization but you didn’t obtain it beforehand, your claim may be denied. You may be responsible for paying the full cost of the service. It’s always best to check whether a service requires authorization before receiving it.
3. **Q: Can my primary care physician (PCP) request an authorization for me?**
**A:** Yes, your PCP can request an authorization for you. In fact, it’s often recommended that your PCP be involved in the authorization process, as they have a comprehensive understanding of your medical history and needs.
4. **Q: What if I need a service urgently and don’t have time to wait for authorization?**
**A:** In emergency situations, you don’t need to obtain prior authorization. However, it’s important to notify Aetna Better Health as soon as possible after receiving emergency care.
5. **Q: How do I know if a particular service requires authorization?**
**A:** You can check your Aetna Better Health plan documents, contact member services, or ask your healthcare provider whether a particular service requires authorization.
6. **Q: What if I have a question about the authorization form that isn’t answered in this guide?**
**A:** If you have a question about the authorization form that isn’t answered in this guide, contact Aetna Better Health member services for assistance.
7. **Q: Is there a way to expedite the authorization process?**
**A:** In certain situations, such as when there is an urgent medical need, you may be able to expedite the authorization process. Contact Aetna Better Health member services to inquire about expedited processing.
8. **Q: What documentation is typically required to support an authorization request?**
**A:** The documentation required to support an authorization request can vary depending on the type of service being requested. Generally, you will need to provide medical records, physician notes, and test results that justify the medical necessity of the service.
9. **Q: If my authorization is approved, how long is it valid for?**
**A:** The validity period for an approved authorization can vary depending on the type of service. Check the authorization approval notice to determine the expiration date.
10. **Q: Can I request an authorization for a service that I already received?**
**A:** Generally, you cannot request an authorization for a service that you have already received, unless it was an emergency situation. Prior authorization is typically required before the service is rendered.
Conclusion: Empowering You to Navigate Your Healthcare Journey
Understanding the Aetna Better Health authorization form for Louisiana is essential for accessing the healthcare services you need. By following the guidelines and tips outlined in this comprehensive guide, you can navigate the authorization process with confidence and ease. Remember to work closely with your healthcare provider, utilize Aetna Better Health’s resources, and advocate for your healthcare needs. We hope this guide has provided you with the knowledge and tools you need to successfully navigate your healthcare journey with Aetna Better Health of Louisiana. If you have further questions or need additional assistance, don’t hesitate to contact Aetna Better Health member services or consult with your healthcare provider. Share your experiences with the Aetna Better Health authorization form for Louisiana in the comments below to help others navigate this process more effectively.
